How the CARES Act Forgot America’s Most Vulnerable Hospitals

![]()
How the CARES Act Forgot America’s Most Vulnerable Hospitals – A federal economic relief package passed by Congress in March promised to provide a lifeline for hospitals, particularly those in rural communities where many facilities struggled to survive even before the coronavirus pandemic.
But over the past 10 months, the distribution of more than $100 billion in CARES Act funding for health care providers has been plagued by a dizzying rollout and, at times, contradictory guidelines for how to use the funding.The result has been a patchwork of problems for rural hospitals, which were already at far greater risk of closure than other health care facilities and in dire need of help, The Frontier and ProPublica found. The scope of those problems is clearly visible in Oklahoma, which tied for the third-highest number of hospital closures in the country in the nine years before the pandemic.
One hospital used more than $1 million in federal aid to pay off its years-old debt to a management company that left before Oklahoma’s first coronavirus case was diagnosed, a potential violation of federal guidelines that could require the hospital to return the money, according to experts.
Three Oklahoma hospitals that were purchased last year after filing for bankruptcy were unable to access more than $6 million in funds deposited by the Department of Health and Human Services, the agency in charge of the rollout for health care providers. The money was instead deposited into accounts tied to the previous owners, leaving the new owners with few options as they tried to keep the facilities from becoming insolvent.
And administrators at yet other hospitals have left millions in relief aid untouched, spiraling deeper into debt for fear that the wrong decision could force them to return money.
“Every day we have new rules, new guidelines, and it’s a struggle,” said Shelly Dunham, CEO of Okeene Municipal Hospital in western Oklahoma. Dunham said she used only $50,000 of the $3 million the hospital received in April and May because of concerns that the facility would have to return the money. “I can’t say we need more money right now. We just need to be able to keep what they’ve given us.”
Under the CARES Act, funding can be used to prevent, prepare for and respond to the coronavirus or to help with expenses or losses caused by COVID-19. The problem is in the details, which Congress left to HHS.
HHS has primarily managed concerns by publicly releasing responses to more than 100 frequently asked questions. Those responses have sometimes contradicted previous guidance from the agency, leaving health care providers confused about how money can be used and what the agency would seek to claw back. The whipsawing guidance has covered a range of topics, including how health care providers could calculate losses from the pandemic and whether they could use the money to pay for long-term capital improvement projects such as new heating, ventilating and air conditioning systems.
“Hospitals’ challenge right now is keeping their doors open and paying their debts,” said Carrie Cochran-McClain, vice president of government affairs and policy for the National Rural Health Association. “There is not enough flexibility to help providers really use the funds as Congress intended for the kinds of things that they need to address for COVID.”
Rural hospitals across Oklahoma and the country are disappearing at an alarming pace that could hasten without help from the federal government, Cochran-McClain said. In 2019, the year before the coronavirus pandemic, rural hospital closures reached a record high, with 18 nationwide. Texas led the country with three closures. Tennessee, Kansas and Oklahoma followed with two each.
Last year, despite the infusion of federal funding, another 17 rural hospitals shuttered, bringing the total number of closures since 2005 to 176.
Unlike larger, wealthier facilities, rural hospitals often have only a few weeks’ worth of cash on hand to operate with. Experts have warned that even with the federal relief aid, many hospitals would struggle. But without it, they would surely fail.

“There was a tussle between the desire early on to get funds out quickly into the hands of people and providers who need it first, and also a compelling need to have oversight of where the money is going,” said James Cosgrove, health care director for the Government Accountability Office. After the first distribution of $50 billion in April, the GAO found that the federal government had sent $558,000 to four closed hospitals that either declined or returned the money.
The Frontier and ProPublica found six other hospitals that closed in 2019 but received more than $3.2 million combined in federal relief payments. More than half of the money went to a hospital in Ellwood City, Pennsylvania, that closed in December 2019 after state inspectors found unsafe conditions for patients.
The relief money was being used for security and to respond to medical records requests until Ellwood City Medical Center could be sold, a bankruptcy trustee said in a December 2020 court filing. The trustee did not respond to requests for comment.
An HHS official said the agency is “in the process of recovering payments” from hospitals that permanently closed before Jan. 31, 2020, but would not say how much it was pursuing or identify any closed facilities that had received aid. Officials said they could not comment specifically on the six hospitals identified by The Frontier and ProPublica because the agency does not release information on individual facilities.
The distribution of funding for health care providers is just one example of complications with the sweeping $2 trillion CARES Act. More than $174 billion in temporary tax breaks benefited mostly wealthy people and large companies. The Paycheck Protection Program, another effort aimed at helping small businesses stay afloat, drew widespread criticism after large companies, including the restaurant chains Ruth’s Chris and Shake Shack, qualified for loans, while smaller struggling businesses were shut out. Ruth’s Chris and Shake Shack later agreed to return the money.
The hospital rescue program similarly helped wealthier facilities pad their bottom lines, while poorer hospitals struggled. In the first round of funding, wealthier hospitals received a larger share of the $50 billion than poor and rural hospitals, according to a report from the Kaiser Family Foundation, a health policy research organization. The report found that those hospitals with a larger share of revenue coming from private insurers received about $44,000 per bed, while poor, rural hospitals got about half that amount.
Subsequently, HHS set aside billions more for rural health care providers and for hospitals with a higher percentage of COVID-19 patients. But that wasn’t enough to make up for the inequities, said Karyn Schwartz, a senior fellow for Kaiser.
“I think they (HHS) were under a lot of pressure to do it quickly, and so they prioritized a quick and simple formula over really targeting the money towards the providers who might be most vulnerable,” Schwartz said.
HHS officials said they have repeatedly made improvements to the system in response to feedback from Congress and health care providers. The agency has changed the way it distributes money, seeking a formal application instead of releasing funding to all hospitals. A new $900 billion pandemic relief package passed in December also gave hospitals more flexibility in calculating revenue losses from the pandemic.
“HHS has balanced the need for flexibility in use of funds to stabilize the health care system with program integrity requirements and the responsible use of taxpayer dollars,” the agency said in a statement released before President Joe Biden took office.
“We’re Doomed”
As rural communities across Oklahoma began experiencing an uptick in COVID-19 cases, the new owner of the only hospital in the small Oklahoma town of Prague fought for access to part of $3.2 million in federal relief aid.
The Prague Community Hospital was one of three that in June asked U.S. Bankruptcy Court Judge Joseph Callaway to help them solve what appeared to be an intractable problem.
The facilities, which included the Fairfax Community Hospital and the Haskell County Community Hospital, were among 11 that entered bankruptcy in 2019 amid accusations that the company that owned them, EmpowerHMS, had engaged in fraud. In a federal indictment unsealed in June, prosecutors accused the company’s owner, Jorge Perez, and nine others of a scheme that allowed rural hospitals to bill at higher rates for blood and urine tests performed elsewhere. The case is set to go to trial in September 2021. Perez and eight other defendants have pleaded not guilty. A tenth defendant has not yet appeared in court.
Each Oklahoma hospital owned by the company was auctioned off by a bankruptcy trustee in charge of settling financial debts incurred under EmpowerHMS.
After unexpected revenue losses from the pandemic, the new owners banked on federal funding from the hospital relief package. But when the money was dispersed, they got nothing.
HHS had instead deposited a total of $6.4 million into accounts connected to the hospitals’ previous owners and managed by bankruptcy trustee Thomas Waldrep.
Since federal rules prevented the money from being transferred, it had to be returned to HHS, Department of Justice attorney Michael Quinn said during a June bankruptcy court hearing.
The new owners would have to wait for another round of relief, Quinn said. Even then, they may not qualify because the money was distributed using the hospitals’ 2019 tax identification numbers and none of the current owners controlled the facilities at the time.
“This is not specific to this case, this is a response to an enormous program of unprecedented size that rolled out billions of dollars on an emergency basis to provide relief and used estimated data to get the money out the door as fast as possible,” Quinn said during the court hearing. “As soon as that happens though, that creates an expectation that, in some cases, the money will not go and land in the correct place. And here, it happened to land in the middle of a corporate sale of an asset.”
Waldrep, the bankruptcy trustee, later said in an interview that he believed the new owners should get a portion of the relief aid but he was hamstrung by the federal rules. The trustee also wanted to use a portion of the money to pay some of the hospitals’ debts from before the sale, including his fee and charges from the management company that operated the facilities during the transition.
“This puts our clients in a very bad position in terms of the continued delivery of care in these very critical needed areas,” Hugh Robert, an attorney for Transcendental Union with Love and Spiritual Advancement, said during the hearing. The Tulsa-based nonprofit that purchased the Prague Community Hospital in May.
Attorneys for the new owners of the three hospitals and for Waldrep asked the judge to allow them to use the money despite objections from the federal government. During the hearing, Callaway grew increasingly irritated at what he viewed as the federal government’s failure to help the clearly struggling hospitals.
The lack of guidance and flexibility from the federal government endangered hospitals instead of helping communities keep them open, Callaway said.
“We don’t do things like this around here,” he said. “All I hear are reasons from the government of why it can’t be done, instead of reasons why it can be done.”
The judge eventually allowed Waldrep to reach agreements with the hospitals. As part of the final plan, Waldrep could use about $750,000 to pay his fees and expenses for overseeing the bankruptcy cases. He would use another $1.4 million to pay Cohesive Healthcare Management and Consulting, which operated the hospitals in bankruptcy.
Some of the money would also go to expenses that were incurred before the sale but were directly related to COVID-19.
The Fairfax and Prague hospitals would each then receive a portion of the remaining $4 million. But because the federal government threatened to later take back money it determined was misused, the hospitals would have to obtain a line of credit that would protect the previous owner from any collection attempts.
Dr. Vishal Aggarwal, who founded the nonprofit that purchased the Prague hospital, said he was never able to secure the financing that would serve as collateral because of the facility’s poor financial state.
“If a second wave hits us, we are doomed,” Aggarwal said in an interview.
Coming to Collect
During the pandemic, hospitals were forced to forgo elective surgeries and other nonessential services that help drive the minimal revenue that rural facilities bring in annually. The losses, coupled with the added costs of preparing hospitals for the pandemic, heightened the urgency of obtaining federal relief.
Some Oklahoma rural hospitals received federal relief aid before the coronavirus pandemic spread to their small towns and immediately began using the money without considering how expenses could later be justified.
In May, Cimarron Memorial Hospital, in the Oklahoma Panhandle, was two weeks away from closing. It had fallen behind on state taxes and was working to settle a lawsuit filed months earlier by the electric company after the hospital failed to pay its several bills. It also owed $1.2 million in past-due fees to NewLight Healthcare, a management company that ran the hospital for nearly a decade before abruptly departing in January 2020.
The hospital received $3.5 million in federal relief payments and loans.
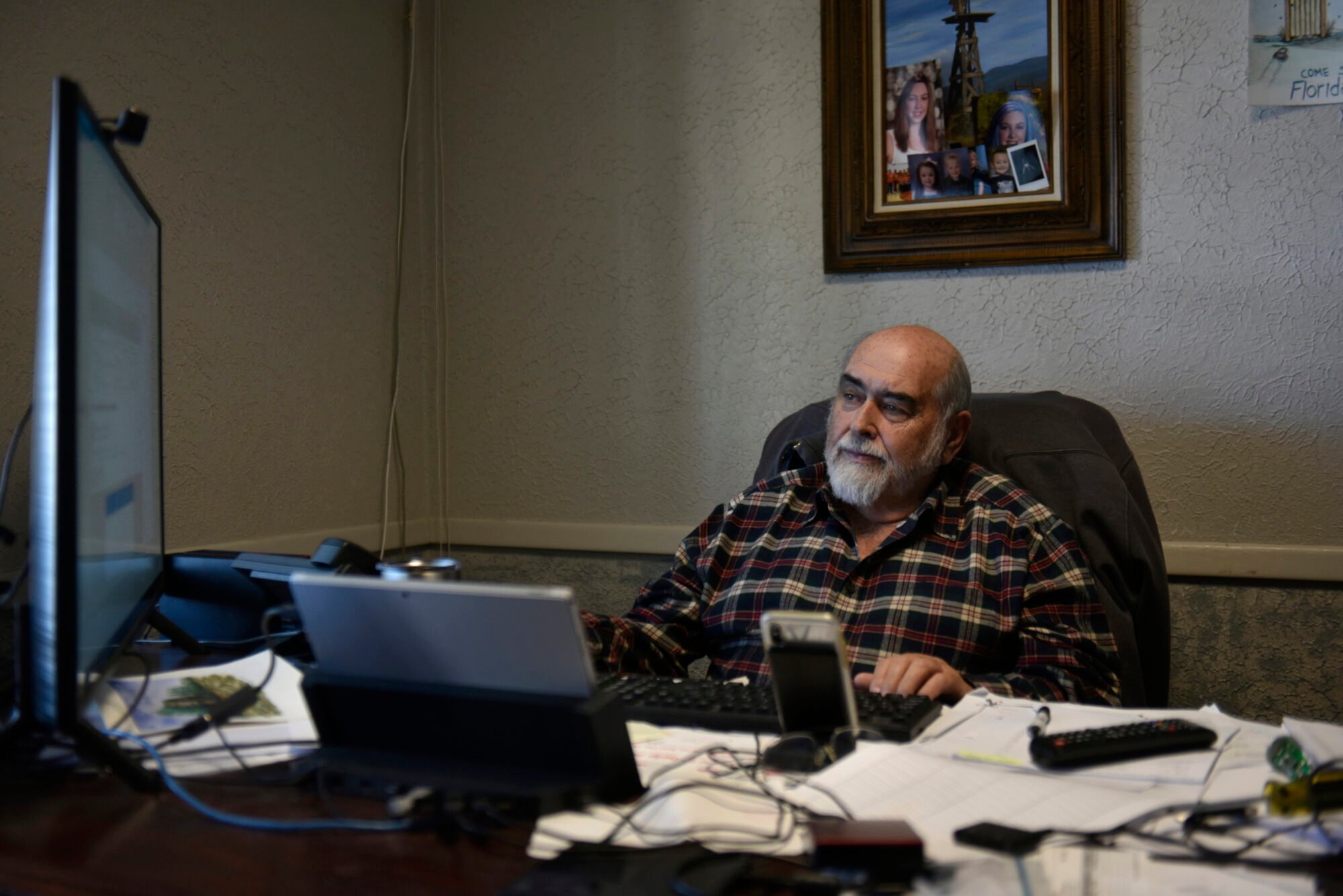
Tim Beard, Cimarron’s chief executive officer, used nearly a third of the relief aid to pay off NewLight Healthcare, a decision that experts say could force the hospital to repay the federal government. HHS has called it “highly unusual” that the relief aid could be used for expenses incurred before Jan. 1, 2020.
For nearly a decade, NewLight provided loans to the Cimarron hospital and deferred management fees, under a contract that allowed it to charge interest on the past-due amounts. The company then placed a lien on the hospital’s incoming payments. If NewLight chose to enforce the lien, as it had already done in another Oklahoma town, the hospital would be required to pay the company before it paid employees or covered bills for medical supplies.
Lee Hughes, an executive vice president for NewLight, declined an interview and did not respond to detailed written questions. In a statement, Hughes said that the company acted in good faith by settling for less than what it was owed.
“NewLight did this both to resolve all past indebtedness owed by the hospital, but also as a gesture of good will,” Hughes said.
The hospital had run out of options to settle its debts, said Beard, adding that he believed there were no restrictions on the coronavirus relief money.
“If I didn’t do things as I should have then we will pay the price for that but we got the community taken care of for eight months longer than we were looking at,” Beard said in an email.
Hospitals will be required to start reporting how they spent the federal relief aid, but HHS officials said no deadline has been set. Those that received at least $750,000 must undergo audits that HHS will use to determine whether money must be returned.
“I think there’s probably many in the industry optimistic that the government doesn’t want to recoup this money, and they’re going to come up with a way to allow the hospitals to keep it,” said Eric Shell, a rural hospital finance expert with the health care consulting firm Stroudwater Associates.
By the time COVID-19 arrived in Cimarron County, the hospital had already used $2 million in federal funds. Aside from the payment to NewLight, Beard said he used $250,000 to replace the hospital’s broken CT scanner, $81,000 to settle its debt to the electric company and another $750,000 to cover payroll and other bills.
The hospital still has $1 million in provider relief funds, according to Beard, who did not provide detailed financial records requested by The Frontier and ProPublica. Beard said he hadn’t compiled the information because it doesn’t have to be reported to the federal government until this year.
“If they take back the money or what we have in savings, we won’t survive,” Beard said in an email to The Frontier and ProPublica.
Another Shot at Relief Funding
Despite vastly different problems with the rollout of the federal program, hospital administrators share a fear that money they thought would save them could now accelerate their closure.
This month, Dunham started using more of the $3 million she had been holding on to. The hospital, she said, needs the money. But Dunham said she hasn’t stopped worrying about the crushing financial situation the hospital will face if the federal government disagrees with how the money is spent and asks for it to be returned.
The Prague hospital has now changed hands. City officials who purchased the hospital this month for $1.3 million say they are not concerned about whether the government will claw back federal funds. Instead, they’re worried about getting access to the money in the first place.
The 25-bed hospital has been operating at or near capacity since Thanksgiving, when Oklahoma experienced a spike in COVID-19 cases that continues to grow. The city loaned the hospital $236,000 from its emergency reserves to pay employee salaries in November and December, according to city officials. And the hospital still needs to make various improvements, including replacing an antiquated system that supplies oxygen to patients.
Prague’s mayor, Cliff Bryant, acknowledged the risk the city took in buying the hospital, given the facility’s history of financial problems and the additional pressures from the ongoing pandemic. But, he said, the move was necessary to ensure residents had access to quality health care.
“It’s either that or shut it down, so it’s not a real good choice,” Bryant said.
Bryant said the city plans to apply for another round of relief money, probably early this year, but he worries about another denial. HHS has an estimated $24 billion left to allocate. The agency has not released details about which providers will qualify and how much they will receive.
Meanwhile, the $1.7 million in relief money intended to help the Prague hospital weather the pandemic is still sitting in a bank account controlled by the bankruptcy trustee. He’s unsure what will happen to the money.
“I think one possibility is that it would just get sent back to the government,” Waldrep said.
How the CARES Act Forgot America’s Most Vulnerable Hospitals
![]()





Responses